‘They Like When They Get to Pepper Spray Us’
Incarcerated people of color with mental illness get less treatment and more solitary confinement.


Group therapy cages for inmates at Mule Creek State Prison near Sacramento. Photo via U.S. District Court, Eastern District of California
During Tashon’s incarceration, prison staff used one word so often to describe him that it became routine.
He heard it while having a breakdown in his cell. He heard it when he requested an appointment with a psychologist or asked to be sent to the Psychiatric Observation Center (POC). He heard it from the mental health professionals who he said treated him like “a nuisance.”
“The correctional officers and the psychologists at all four [prisons I’ve been in] accused me and other Black brothers with mental illnesses of just being assholes,” Tashon wrote in a letter to Solitary Watch.
“A lot of times they won’t send us to POC, but strip us naked, take all our clothes, blankets, mattresses, and leave us in our cells cold and naked and sleeping on steel bunks. They do this as punishment for acting, in their words, like an asshole.”
The letter exposed a problem that is often ignored by those who are concerned about prison conditions.
In jails and prisons throughout the country, people with mental illness of all races suffer mistreatment and medical neglect, and have high rates of suicide and self-harm. But people of color with mental health disabilities are even less likely to receive proper mental health services.
Often treated with disrespect, they are disproportionately punished and placed in solitary confinement, which has been shown to exacerbate mental illness.
Tashon’s story is an example of how this mistreatment coincides with systemic racism behind bars, with devastating consequences
Tashon, who asked that his full name be withheld to avoid repurcussions, is a Black man with PTSD, bipolar disorder, and anxiety, who bounced around several prisons in Pennsylvania, including the maximum-security SCI-Greene, as well as SCI-Fayette, SCI-Houtzdale, and SCI-Somerset.
At every prison, he felt he has was targeted for his race and mental health disability by correctional officers and healthcare workers.
“A lot of us get mad easily, act out quickly, and go straight to hurting ourselves, so the correctional officers will antagonize us, refuse us food, etc,” he wrote. “They like when they get to pepper spray us.”
Treatment Bias
Throughout his time in prison, Tashon noticed that this disturbing treatment was particularly directed towards Black individuals with serious mental illnesses. In his view, white people with mental health disabilities are taken more seriously, and shown a higher degree of sympathy for their situations, while Black people are more likely to be viewed as “passive aggressive” and disciplined for their behavior.
On the rare occasion that Black individuals get to see a psychologist, he wrote, they are “disrespected,” “talked over,” and diagnosed with behavioral issues.
“Whites are diagnosed with more legitimate and sympathetic diagnoses and they’re sent to mental health units,” Tashon claimed. “We’re sent to behavior modified units and security modified units which offer no mental health treatment, only punishment.”
It shouldn’t be surprising that systemic racism in the U.S. extends to inequalities of access to mental health services in the communities that many incarcerated people come from.
According to a 2001 U.S. Surgeon General’s report on mental health, racial and ethnic minorities have limited access to mental health care due to barriers like the cost of health insurance and geographic distribution.
As the report outlined at the time, nearly one-fourth of African Americans and 37 percent of Latinos were uninsured, significantly higher than the rate among whites. Although the Affordable Care Act helped decrease uninsured rates across the board, a 2019 analysis found that 11.4 percent of Black people and 20 percent of Hispanics were uninsured—and that, in fact, uninsured rates had slightly risen since a low in 2016.
Without insurance, the cost of seeing a psychiatrist or psychologist is often unaffordable; even those on Medicaid can have trouble finding providers who accept their insurance or offer services to high-need clientele.
In addition, the availability of mental health services depends on where one lives. For example, a large percentage of African Americans live in the rural South, where there is a low concentration of mental health professionals.
Lack of Diagnosis
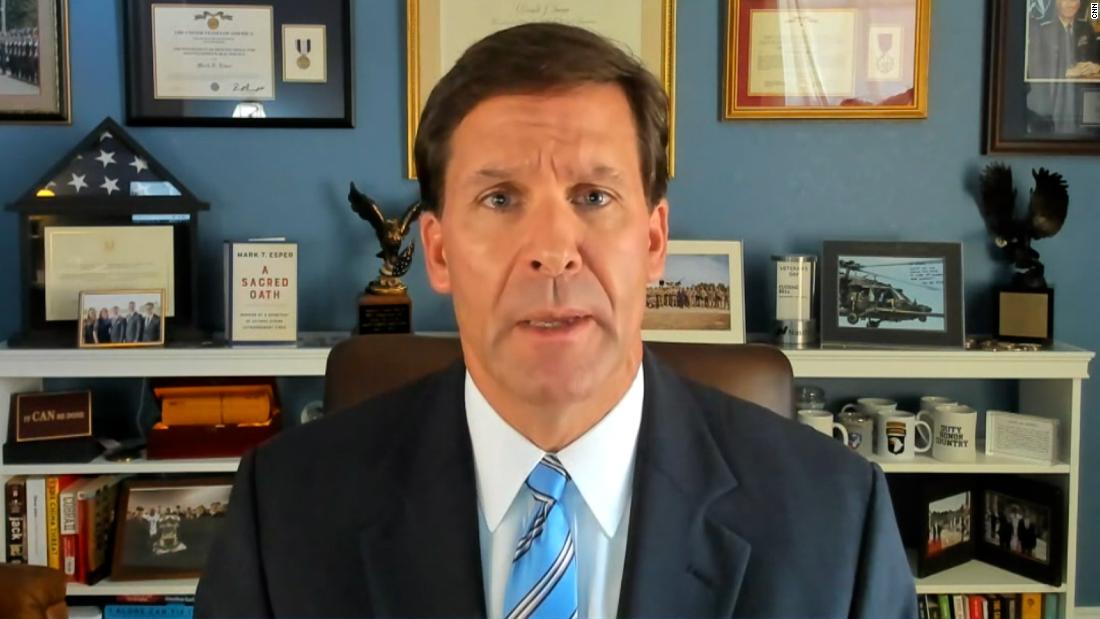
These problems of access mean that when people of color are arrested, they are less likely to have a preexisting, professional diagnosis of a mental illness, Terry Kupers, a psychiatrist and expert on the psychological impacts of incarceration and solitary confinement, told Solitary Watch.
During jail intake procedures, staff who are performing screenings may ignore familiar symptoms of mental illness, or prejudicially believe that mental health treatment will not be effective for people of color.
This racial bias often prevents people of color from qualifying for diversion programs that could keep them out of jail altogether, as well as for adequate mental health treatment inside correctional facilities.
These individuals instead are more likely to be placed in general population in their local jails, where the psychological toll of overcrowding and violence can cause further anxiety, says Kupers.
In a 2014 letter outlining problems in Los Angeles County jails, the Department of Justice noted that the “cramped and crowded” conditions “create an environment that may contribute to prisoners’ mental distress.”
According to Kupers, when people with mental health disabilities end up in this environment, they often don’t know how to react, act out, and are punished by correctional officers for their inability to deal with the stress.

Terry Kupers. Photo courtesy University of California.
This punishment often includes solitary confinement, where, according to Kupers, many individuals experience their first psychotic episode.
Even while experiencing a psychological crisis behind bars, people of color have to wait disproportionately longer than their white counterparts before they are diagnosed with a mental health disorder.
A New York City Department of Health and Mental Hygiene study shows that non-white mental health patients in the city jail system were more likely to have waited seven days or more after admission before receiving their diagnoses.
In addition, among the pool of individuals whose diagnoses took longer than seven days, close to 40 percent of Blacks and 26 percent of Latinos experienced solitary confinement, while only about nine percent of whites did.
Punishment First, Professional Help Second
Black and Latino individuals with mental health disabilities are more likely than whites to be punished with solitary confinement. On New York’s Rikers Island, Black people are sent to punitive segregation at 5.7 times the rate of white people—and admitted into the mental health units at just 0.6 times the rate of white people.
This is true throughout the New York City jail system, where non-Hispanic Blacks and Hispanics with serious mental illnesses are about 2.5 and 1.7 times more likely to enter solitary confinement than whites, according to a report by the Vera Institute of Justice.
It is also more common for non-white individuals to stay longer in solitary confinement.
“In the same general situation of a prisoner breaking a rule and suffering from an emotional difficulty, the white prisoner is most likely to be sent to mental health treatment and the Black prisoner or Latinx prisoner is likely to be sent to solitary confinement,” said Kupers.
As law professor Andrea Armstrong explains in her article Race, Prison Discipline, and the Law, a groundbreaking 1980 statistical analysis found that Black and white individuals are equally likely to engage in rule-breaking activity, but correctional officers are more likely to report a rule violation if the individual is Black.
This racial disparity likely stems in part from implicit biases Americans have regarding race.
In a series of implicit association tests, participants more quickly associated the word “bad” with Black or darker skin, and “good” with white or lighter skin. Participants were also more likely to falsely identify an item as a weapon when it appeared on screen alongside a Black face, compared to a white face.
In a prison or jail setting, these biases can be amplified by racial disparities among staff. In 2005, Latino and Black people made up more than three-quarters of people incarcerated in New York state prisons, but held less than a quarter of correctional staff positions.
These assumptions of wrongdoing and criminality leads to non-white individuals generally being treated with much more hostility than their white counterparts.
Retaining White Privilege Behind Bars
This research reflects the experiences of Jerome Wright, a Black activist formerly incarcerated at Elmira Correctional Institution in Upstate New York. In his view, when white people enter prison, they retain their white privilege.
While incarcerated individuals are treated poorly by prison staff across the board, white people don’t face the same struggles in prison as Black and Latino people—who are treated with more disrespect, are more likely to be assaulted, and overall, have a more difficult experience, according to Wright.
Black and Latino individuals with mental health disabilities are also targets of verbal and physical attacks from correctional officers. One study found that in Los Angeles jails, a third of all deputy-on-prisoner use of force incidents are perpetrated against people with mental health conditions.
Interviewees in this study said that sheriff ‘s deputies “respond more aggressively and more skeptically to requests and actions, including about health concerns, by Black and Latino prisoners as compared to white prisoners, even when it seemed mental health issues underline the conduct.”
This was Howard Morris’ experience while incarcerated both in Pennsylvania and New York. Morris is a Black man who has struggled with his mental health, attempting suicide several times in his past.
He says there is often a noticeable difference between how white and Black people are treated. While he saw white individuals get sent to a special block for the mentally ill, where there was more time out of cell, games, and extra food, he said he and other non-white people were treated with disdain.
“I was targeted because I’m on meds,” wrote Morris in a letter to Solitary Watch. “On shower day they would skip my cell and say I was asleep.”
Wright said that in his experience, the correctional staff always includes “bad apples” who are “the ones who go to [the solitary unit] and abuse people.”
He continued: “These bad apples are the ones who know a guy has a mental health issue and they’ll give him a ticket just to mess with him or will provoke him to act in a way that will be something that he can be written up for.
“It’s not reported on—and if it was reported on, who are you going to believe? The correctional officer, or the guy with a mental health issue who is in prison for a crime?”
Racial Disparity in Medical Diagnoses
Even when Black and Latino patients do manage to receive a mental health diagnosis in jail and prison, the diagnoses themselves often appear to be clouded by racial stereotypes. The Diagnostic Statistical Manual (DSM), the standard classification of mental disorders used by mental health professionals in the United States, categorizes diagnoses into two “axes.”
Axis I contains disorders such as schizophrenia, depression, and bipolar disorder, while Axis II contains personality disorders such as antisocial personality disorder.
According to Kupers, “Because of racism, people of color are more likely dismissed as Axis II.”
In the eyes of many jail and prison medical staff, he added, people of color with mental health issues are not actually ill; they simply have an “antisocial personality” or attitude problem.
This is clear in the New York City Jail system, where non-white individuals are more likely to receive diagnoses of mood, adjustment, or antisocial personality disorders.
As a 2015 study notes: “There is a well-documented social tendency to view non-White persons as criminal or untruthful, which in our mental health setting could lead staff to not detect mental illness or to give a more pejorative diagnostic label when patients exhibit stress from solitary confinement.”
In comparison, the study notes, white individuals are more likely to be diagnosed with mental problems that are generally thought to be more “legitimate,” such as anxiety or depression.
Wright often observed this throughout his time in the New York State prison system.
“Our behaviors are always violent. OCD is a white person’s problem. Black people don’t get that. If we have a problem, it’s violence,” said Wright.
“It’s something that puts us in a position where if a staff member wants to respond violently to you, they can say, ‘This guy has this issue.’ But white guys don’t have these issues. They have anxiety disorders.”
Another obstacle people with mental health disabilities face is the accusation of “malingering,” which correctional medical staff apply to people who they believe are feigning health symptoms for personal gain—for example, to avoid work or punishment, or get out of solitary.
In the Pennsylvania prison system, Morris wrote, “Blacks and Hispanics are treated like we are faking or we are trying to seek attention.”
“The diagnosis of malingering is overutilized with people of color, because given the racism in the institution, there is less compassion, there is less empathy for the emotional pains of people of color,” said Kupers.
“Therefore, they get dismissed as rule violators or the worst of the worst, and they get punished instead of treated.”

Melat Eskender
The dehumanization and demonization that people of color experience in the outside world only intensifies in prisons and jails. For people with mental health disabilities, the impact of this treatment can be devastating—and often doesn’t end with their prison sentence.
Many Black and brown individuals with mental illness are never the same again, said Wright, and return to their communities permanently scarred.
“I’ve had friends who, after they were ‘taken care of’ by the [prison] mental health staff, they were a fraction of themselves,” he said. “They were ghosts.”
This story is published in partnership with Solitary Watch. Melat Eskender, a student at Yale University, is leader of the Fresh Start Program, which helps formerly incarcerated individuals apply to have their criminal records erased. She also serves as facilitator of the Connecticut Reentry Policy Working Group; and as a researcher Yale Law School Prof. Judith Resnik on corrections and state punishment.

 Landwebs
Landwebs